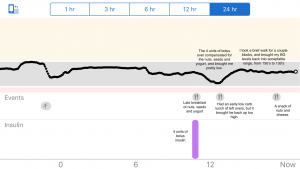
It is a truism that some foods have more carbs than others. The more carbs you eat, the higher your blood glucose can climb. If you’re using insulin, you’ll need more to counteract a heavy dose of carbs.
So the counterpoint can also be valid. Low carb foods can lower the amount of insulin you need.
I’ve adjusted my diet since becoming diabetic to do this. It is much easier to manage my levels when I don’t have huge carbohydrate loads to contend with. I can usually fill up on low carb vegetables (which is healthy in its own regard) and rely on fewer foods that are heavy with carbs.
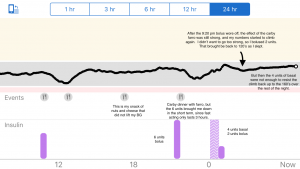
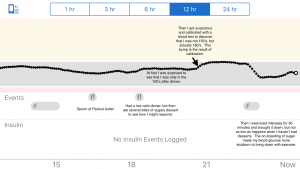
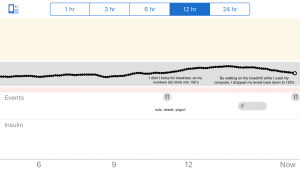
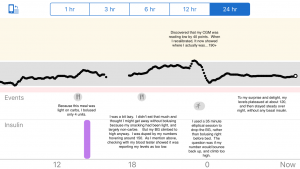
But even if I eat only a seemingly no-carb option, if I eat a lot of it, my sugars will still climb. There is something about being FULL that stresses my system and causes me to struggle to keep my levels low.
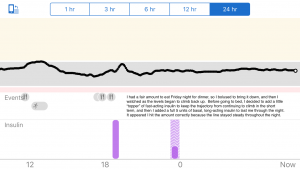
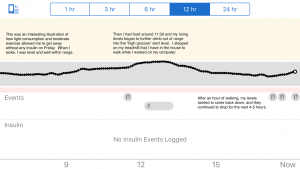
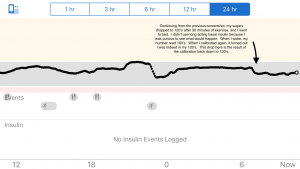
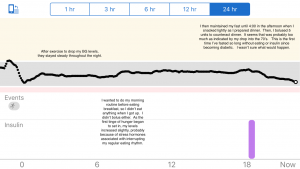
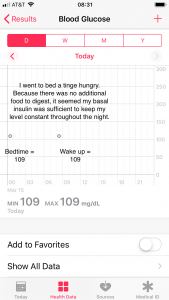
Last night, I had dinner early. It had probably been at least six hours before I went to sleep. I was at 113 when I went to bed, and I was a tad peckish. Rather than eating something, I drank some water to fill the “empty spots” in my stomach. I was curious to see how much my levels would climb over night without any long-acting (basal) insulin.
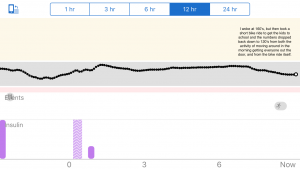
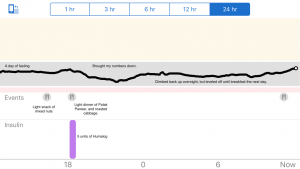
This morning I was at 132. I found that encouraging. It wasn’t a flat line, but it remained within range. Had I gone to bed earlier or had I been better about exercising these last couple days, it might have stayed completely level. That suggests that I’m still producing some insulin, since my nutritionist says the levels would rise rapidly overnight without insulin for someone who has no exogenous insulin production.
The real take-away for me is validity of the old Japanese adage, “Keep your stomach at 8/10th full.” (Hara, hachi-bun me.) Eating too much taxes the system. When I can monitor my blood glucose as I can, I can see the negative, real-time impact of that extra and perhaps unnecessary second or third helping. Eating light is better for controlling blood sugar levels, even if eating no-carb foods.